Dr. Cheyette referred us to Lucille Packard Children’s Hospital at Stanford. Specifically, to a neurosurgeon there, Dr. Cheshier, to discuss possible surgery.
It was a bit upsetting when he first came into the cramped appointment room with two baby docs in tow. Suddenly the room was very crowded, stuffy, and awkward.
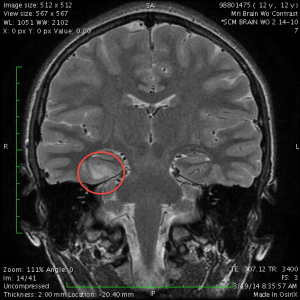
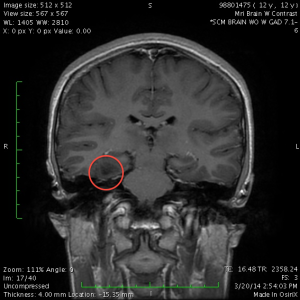
However, Dr. Cheshier’s manner made up for it. He patiently answered all of our questions, showed us the lesion on the MRI images, and talked about what the surgery would be like. He said that although the hippocampus was fairly close to the lesion, he was confident he would be able to resect the lesion without damaging the hippocampus. He said that this surgery had a 70% no-seizures-ever-again success rate, with another 20% chance of greatly reduced need for medication.
He ordered a follow-up MRI in 3 months, to verify that it was not growing.